Help your customers find vetted point solutions that work for their employee population, saving money, providing better care, and driving lasting results.
Once an employee population is integrated into NavMD, you’ll be able to see potential savings with any specific point solution. Once that solution is implemented, we track its success and share ROI insights with you.
Find solutions faster with NavMD.
Identify where your population’s emerging risks are headed and mitigate high-risk claims before they happen.
After you’ve identified a point of interest, our health strategy team facilitates coordination to a vetted solution partner.
Once connected with a solution partner, NavMD will continually monitor and track the performance of the deployed solution to ensure expected success.

NavMD works with thousands of benefit advisors and employers who are in search of proven cost containment strategies. Once you’re built into the NavMD Marketplace, advisors and employers are able to see your potential impact on their plan and connect with you right within our platform.
Once a benefit advisor or employer identifies your solution as a cost containment strategy, a dedicated NavMD team member will educate and qualify the plan for you, saving your sales and marketing teams countless hours of emails, meetings and phone calls.
If your services are a fit for the plan, a NavMD team member will coordinate an introductory meeting to deliver a hot and qualified opportunity right to your team. And once you’re ready to onboard the plan, the data is ready right in our platform.
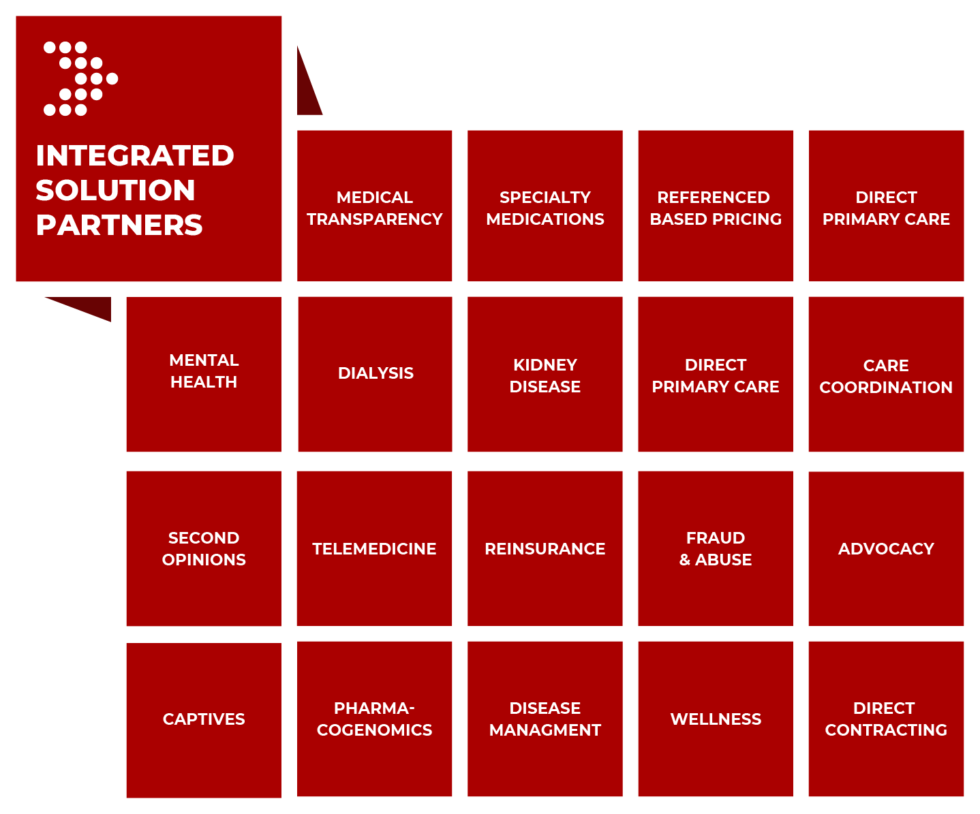
We work behind the scenes to find vetted and proven solution partners for our Marketplace that help save money, provide better care, and drive lasting results – it’s part of our expertise.
Do you have a healthcare solution that could help Benefit Advisors, Employers, and members? Join our growing list of vetted and proven point solutions!
Once integrated into the NavMD platform, users will be able to see potential savings with a point solution. After a solution is implemented, we track success and provide a road map to prove it.